Today I had my telemedicine appointment with my genetic counselor via Zoom. For those of you who aren’t familiar, Zoom is a teleconferencing app that has become really popular during COVID-19. There are some pretty legit security questions with it, but… it is the tool we have at the moment, so… it is what it is.
My genetic counselor’s office reached out to me a few weeks ago to inform me that my appointment would be via Zoom, so I went ahead and downloaded the app at the time. I got an email from my counselors office yesterday, which had the meeting login information, a video to watch on telegenetics appointments, and general tips for having video conferencing appointments.
This is actually my second appointment with a genetic counselor. I met with one about six years ago, but decided against BRCA testing at that time because my health insurance wouldn’t cover it and my husband and I were about to start trying to have our daughter. In addition to breast cancer, the BRCA genetic mutations also have a relationship to ovarian cancer. Unfortunately, the survival rates of ovarian cancer are much different than breast cancer, leading many women to have their ovaries removed upon learning of a BRCA genetic mutation. Since we were about to start a family, I didn’t want that knowledge hanging over my head during that time.
However, it’s been six years and I am now ready to go down the testing path. This is also one of the last things I need to do before going on tamoxifen. Having a negative or a positive result from the testing could possibly raise or lower my breast cancer odds, so it is a useful tool for my doctors and I to have when deciding the preventative path I’ll be taking.
During the appointment, the genetic counselor went through my own personal health history as well as that of my family. Prior to the appointment, I was asked to fill out a family health questionnaire, which goes over who in your family has had cancer in the past. These forms are always a bit hard for me to fill out, as I’m not entirely sure of my mother’s comprehensive health history and I have no insight into the health history of my biological father or his immediate or extended family.
After talking through this, the counselor walked me through recent updates in genetic testing. During my last appointment, BRCA 1 and BRCA 2 were the only genes that they were really testing for. However, since then, there have been findings that other genetic mutations can also have a relationship with breast and other forms of cancer. We also went through a statistic I’ve always found fascinating: out of all the women who get breast cancer, around 80% have no indications they will get it, a smaller percentage (I can’t remember the number, but I want to say around 15%) have a family history, and the remainder, a very small percentage, have a correlation with one of the now-identified genetic mutations. I think it puts preventative techniques in perspective when you realize how many women who will get breast cancer don’t have the warning signs that people like myself have, and yet will still get cancer. I also feel that it goes against the narrative that we are fed on breast cancer and hope that we are able to identify a preventative path for these women as well.
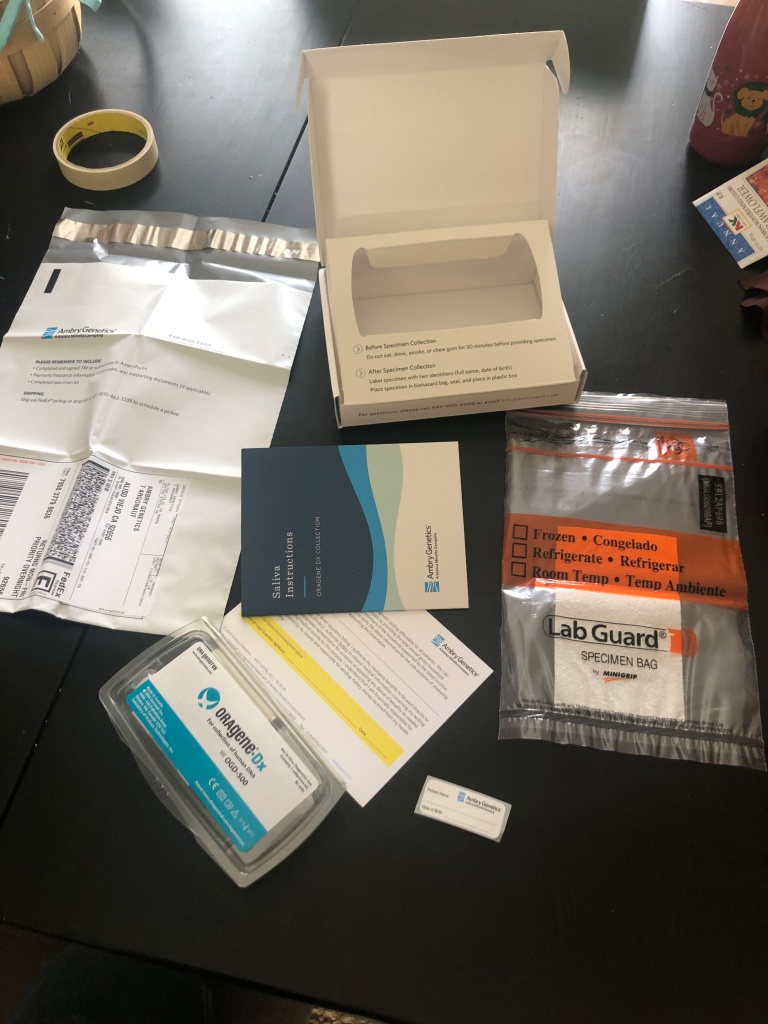
With my counselor’s guidance, I’ve decided to move forward with testing for BRCA 1 and 2, as well as the other genetic mutations that have been identified to correlate with breast and/or gynecologic cancers. To get the testing done, I’ll have to sign some paperwork sent to me by my counselor. She’ll then arrange for the testing company to send me the test, which requires a saliva sample, to my house. I’ll do the test at home and then send it in. The lab will take about 2-3 weeks to do the testing, at which point I’ll get a phone call and/or appointment from my counselor.
My counselor explained that there are three possible results for each genetic mutation. The first is a positive test, which could possibly raise my breast cancer odds, although it could have no impact on my current odds. The second is a negative result, in which case my odds could be lowered, but the models would need to be re-run. The third possible result is similar to that on a non-statistical difference, which is treated as normal human variation and would be treated as a negative result.
We also talked about what to do if I have a positive result. Both my siblings and daughter have a 50% chance of having a positive result if I have a positive result, so we talked about communicating my results with my family members. With my daughter, they like to pick the right time to share this information with minors and then allow them to choose if they want testing after the age of 18. Because different people will react to the information differently, and some people don’t want the information at all, it’s not really fair to make her do the testing before 18, unless it really is her choice.
For now, I’m just waiting to fill out the appropriate forms, get my test in the mail, and spit in a tube! 😛 Good times.